The state of inflammation in the human body tends to worsen gradually over time in a process known as inflammaging which is known to contribute negatively to human health, quality of life and disease risk.
It is also true that the human gut microbiome loses diversity and resilience as we age, a topic I discussed at greater length in an earlier Florastor feature.
These processes, though distinct, are not independent of each other.
The human gut microbiota plays a fundamental role in mediating bodily inflammation and the process of inflammaging because it creates compounds that interact with multiple bodily systems and can influence them in either a pro or anti-inflammatory direction, depending on whether or not it is in a well- balanced state.
Which brings us to the content of today’s article, a deeper exploration of the relationship between inflammation and the gut microbiome and how this relationship is influenced by external factors like diet, lifestyle and probiotic use.
Let’s get to the good stuff.
Inflammation & The Microbiome – A Primer
There are quite a few places we could initiate today’s discussion but I’d like to start with a recently published human study out of the Cell journal which really offers unique insights into this area of inquiry.
In that human trial, the researchers observed that an increased intake of fermented foods like kombucha, kimchi and kefir led to a parallel increase in gut microbiome diversity and a reduction on bodily inflammatory markers.
Fermented foods contain much smaller amounts of healthy bacteria than we’d find from a probiotic supplement, but clearly they can still meaningfully influence gut microbiome diversity – which is a measure of how much and how many different types of helpful bacteria are present in the microbiome.
Here’s why these findings are so relevant for today’s content:
1. Although there is some nuance here, generally speaking good gut bacteria tend to create compounds known as SCFAs [Short chain fatty acids] that have anti-inflammatory influences on the body, whereas “bad” gut bacteria tend to create compounds known as LPS [lipopolysaccharides] that stimulate inflammatory responses within the digestive tract that can affect other tissues.
2. When we have ample amounts of healthy bacteria from many different families (aka microbiome diversity) we enjoy the benefits of these compounds known as SCFAs, which also create an environment in the digestive tract that makes it hard for the “bad” bacteria to thrive and minimizes their influence on our health.
There is even more to it, however.
Let’s use Type 2 Diabetes as an example.
Even though we may not conventionally think of it as an inflammatory condition, chronic inflammation is increasingly considered a strong driver of type 2 diabetes.
Certain inflammatory markers, like TNF-A and adiponectin are strongly connected with diabetes and insulin resistance.
What’s also true is the fact that someone living with type 2 diabetes is more likely than an otherwise healthy person to have imbalances in their gut microbiome – known as dysbiosis.
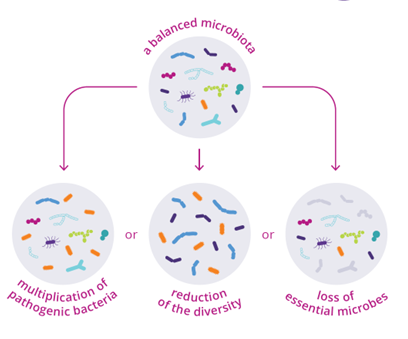
Dysbiosis is a scientific way to refer to a microbiota that has lost overall diversity and likely has harmful quantities of less helpful bacteria, which of course contribute to inflammation as discussed earlier.
And it isn’t just relevant to type 2 diabetes either, there are clear trends that exist between the state of the human microbiome and an individuals health and disease status across multiple conditions.
The polyphenol and fibre content of plant foods (fruits, veggies, nuts, beans, whole grains) and omega-3 content of fish (salmon, sardines, trout) are known to positively influence gut microbiome diversity which is why broad studies show people who eat these foods more tend to have a microbiome profile that features more healthy, anti-inflammatory bacteria.
Let’s take things a step further and examine the role that probiotics like Florastor have to play in contributing to the connection between inflammation and the gut microbiome.
The Anti-Inflammatory Role Of Florastor
Probiotics like Florastor have a meaningful role to play in maintaining and/or restoring a dysbiotic gut to a balance state, particularly after acute events like antibiotic use and infection from pathogenic bacteria like H. Pylori or C. Difficile.
From this perspective, we can think of probiotics as inherently anti-inflammatory – especially since they reduce populations of “bad” bacteria and thus reduce the production of harmful inflammatory LPS compounds discussed earlier.
When we dig deeper into how the S. boulardii probiotic actually works on a cellular level, that understanding is further enhanced.
S. Boulardii is known to secrete various protein compounds that interfere with the flow of inflammatory pathways in the gut while also being capable of directly binding and neutralizing harmful bacteria to stop them from facilitating the creation or harmful inflammatory compounds.
There is also growing interest around the role that S Boulardii plays in increasing the production of beneficial short chain fatty acids like butyrate, which are known to facilitate anti-inflammatory messaging throughout the digestive tract and beyond.
Many digestive and general health issues are characterized by low levels of SCFA production, adding to the intrigue and health value of strategic S. Boulardii use.
When a child has gastroenteritis, the priority is to prevent dehydration. So, it's crucial to ensure the sick child stays well hydrated. Additionally, if we could reduce the duration and intensity of symptoms, we would. In this context, the best thing we can do is give the intestinal microbiota a helping hand in defending us.