Who hasn't taken antibiotics at least once in their life? In 2019 alone in Canada, 207.6 million daily doses were dispensed by community pharmacies and 16.4 million by hospitals, according to a report from the Public Health Agency of Canada.
While antibiotics are an important part of medicine, their overuse and misuse is a concern to health authorities. Not only does this harm vulnerable patients, but it also contributes to increased antibiotic resistance worldwide.
How antibiotics work
There are two main ways in which antibiotics work:
- they prevent the growth and proliferation of bacteria
- they kill bacteria.
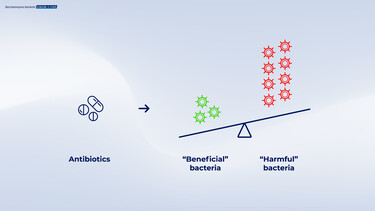
While antibiotics attack the "bad" bacteria that cause an infection, they also harm innocent victims: the "good" microorganisms also die.
Common side effects of antibiotics treatment
About one in five people experience side effects when taking diarrhea, constipation, bloating, abdominal pain, etc.
Here's how it works. To perform its functions and protect us, the intestinal microbiota must be composed of a large number of different species. Their number and diversity are essential to our health. Antibiotics disturb the microbiota! They reduce the number of bacterial species and are associated with the presence of antibiotic resistance genes. These disturbances can last for months or even years after an antibiotic treatment.
Figure 2: Following antibiotics, there is an imbalance in the diversity bacteria in the gut, with an increase in harmful bacteria
In the short term, antibiotics reduce our army of good bacteria. As a result, the mucus layer that helps protect the intestinal wall becomes thinner and the junctions between cells loosen. In other words, antibiotics weaken the intestinal wall. This results in diarrhea until 35% of cases in children, and until 39% in adults. Antibiotic-associated diarrhea (AAD) can occur during treatment and up to 8 weeks after treatment is stopped.
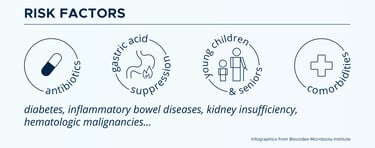
It varies according to age, individual susceptibility, and antibiotic category:
Preventing or reducing adverse effects is possible
Several scientific studies have shown that specific strains of probiotics help limit the damage caused by antibiotics. They help fight pathogenic bacteria and promote a good immune response.
Since probiotics composed of bacteria are likely to be killed by antibiotics, it is beneficial to choose probiotics composed of yeast. Florastor is the only probiotic supplement containing the yeast Saccharomyces boulardii CNCMI-745, a strain naturally resistant to all antibiotics. This means that you can consume our probiotics without having to worry about taking antibiotics 2-3 hours apart (minimum).
Saccharomyces boulardii CNCMI-745 has been researched worldwide for over 65 years. Florastor probiotic supplements have been studied in over 100 clinical trials and have been used for 65 years. Florastor reduces the incidence of antibiotic-associated diarrhea by up to 80% in children and up to 84% in adults.
It promotes the balance of the intestinal microbiota and strengthens the immune system. Saccharomyces boulardii CNCM I-745 has been recommended by :
- The Canadian Digestive Health Foundation (CDHF)
- The World Gastroenterology Organization (WGO)
- The European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN)
It's hard enough to fight off infections without suffering adverse effects from antibiotic treatment. Probiotic supplements such as Florastor are our allies.
- Tyler Yan Ran D. et Goldman (2020) Probiotics for antibiotic-associated diarrhea in children. Canadian Family Physician Vol 66: 37-39
- Jaime Ramirez, Francisco Guarner, Luis Bustos Fernandez, Aldo Maruy, Vera Lucia Sdepanian et and Henry Cohe (2020). Antibiotics as Major Disruptors of Gut Microbiota. Frontiers in Cellular and Infection Microbiology . Vol 10, article 572912
- Guo Q, Goldenberg JZ, Humphrey C, El Dib R, Johnston BC. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No.: CD004827.
- Agence de la santé publique du Canada. Rapport du Système Canadien de Surveillance de la Résistance aux Antimicrobiens https://publications.gc.ca/collections/collection_2022/aspc-phac/HP37-21-2021-fra.pdf
- Radio-Canada. (2017) Surutilisation d’antibiotiques au Canada, selon une étude. Tiré de : https://ici.radio-canada.ca/nouvelle/1066443/surutilisation-ordonnance-antibiotiques-canada-institut-information-sante-icis
- Fondation canadienne de la santé digestive. Faut-il prendre des probiotiques pendant la prise d’antibiotiques ? Consulté le 15 décembre 2022 https://cdhf.ca/fr/faut-il-prendre-des-probiotiques-pendant-la-prise-dantibiotiques/
- Gibson MK, Crofts TS et Dantas G (2015) Antibiotics and the developing infant gut microbiota and resistome. Curr Opin Microbiol 1-12.
- Jakobsson HE, Jernberg C, Andersson AF, Sjölund-Karlsson M, Jansson JK et Engstrand L (2010) Short-Term Antibiotic Treatment Has Differing Long-Term Impacts on the Human Throat and Gut Microbiome. PLoS ONE 1-12.
- Jernberg C, Löfmark S, Edlund C et Jansson JK (2010) Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology 3216-3223.
- Neut, C., Mahieux, S., & Dubreuil, L. J. (2017). Antibiotic susceptibility of probiotic strains: Is it reasonable to combine probiotics with antibiotics? Medecine et maladies infectieuses, 47(7), 477-483.
- Hickson M et al. Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial. BMJ 2007; 335: 80
- Klein, S.M., Elmer, G.W., McFarland, L.V., Surawicz, C.M., & Levy, R.H. (1993). Recoveryand eliminationof the biotherapeuticagent,Saccharomyces boulardii, in healthyhumanvolunteers. Pharmaceutical Research,10, 1615-1619.

.jpeg?sw=375&sfrm=jpg&q=90)